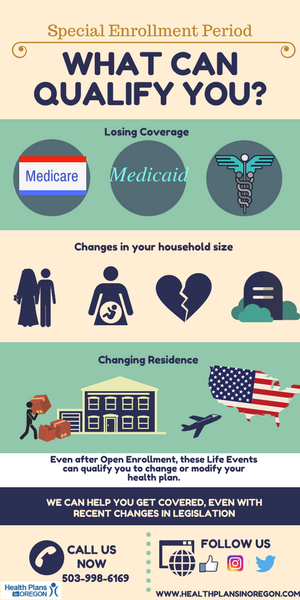
Are you still able to enroll under certain life events or special enrollment period?
Annual Open Enrollment Period is over but you may still able to enroll on a qualified health plan or change your health insurance. Here are some circumstances that may allow you to still enroll:
1. Lost of health insurance coverage:
Losing:
- job-based coverage
- COBRA coverage
- individual health coverage for a plan or policy you bought yourself
- eligibility for Medicaid or CHIP
- eligibility for Medicare
- coverage through a family member
2. Changes in household size
If you or anyone in your household in the past 60 days have these type of life events:
• Got married. Pick a plan by the last day of the month and your coverage can start the first day of the next month.
• Had a baby, adopted a child, or placed a child for foster care. Your coverage can start the day of the event — even if you enroll in the plan up to 60 days afterward.
• Got divorced or legally separated and lost health insurance.Note: Divorce or legal separation without losing coverage doesn’t qualify you for a Special Enrollment Period.
• Death. You’ll be eligible for a Special Enrollment Period if someone on your Marketplace plan dies and as a result you’re no longer eligible for your current health plan.
3. Changes in residence
• Moving to a new home in a new ZIP code or county
• Moving to the U.S. from a foreign country or United States territory
• A student moving to or from the place they attend school
• A seasonal worker moving to or from the place they both live and work
• Moving to or from a shelter or other transitional housing
4. More qualifying changes:
• Changes that make you no longer eligible for Medicaid or the Children’s Health Insurance Program (CHIP)
• Gaining membership in a federally recognized tribe or status as an Alaska Native Claims Settlement Act (ANCSA) Corporation shareholder
• Becoming newly eligible for Marketplace coverage because you became a U.S. citizen
• Leaving incarceration
• AmeriCorps VISTA members starting or ending their service